Blood Vessels
Blood Vessels and Their Structure
🔄 General Function of Blood Vessels
-
Blood vessels form a closed circuit for blood to circulate throughout the body.
-
Oxygen-rich blood is pumped from the left side of the heart, travels to all body cells, and returns oxygen-poor blood to the right side of the heart.
🛤️ Types of Blood Vessels
Blood travels through the following vessels in order:
-
Arteries – carry blood away from the heart.
-
Arterioles – smaller branches of arteries.
-
Capillaries – the smallest vessels where exchange of gases and nutrients occurs.
-
Venules – small veins collecting blood from capillaries.
-
Veins – carry blood back to the heart.
🧠 Arteries: Structure & Types
Arteries are classified based on size and wall structure into:
| Type | Key Features |
|---|---|
| Large (Elastic) | Rich in elastic tissue. Example: Aorta. |
| Medium (Muscular) | Rich in smooth muscle. Example: Coronary arteries. |
| Arterioles | Smallest arteries, control blood flow into capillaries. |
🧱 Arterial Wall Structure (All arteries have 3 layers)
1. Tunica Intima (Inner layer)
-
Endothelium: A thin layer of flat cells lining the inside of the artery. Helps regulate blood flow and prevents clots.
-
Subendothelial tissue: Loose connective tissue, contains collagen, elastin, and other structural proteins.
-
Internal Elastic Lamina: A thin elastic sheet that allows the artery to stretch.
2. Tunica Media (Middle layer)
-
Thickest layer.
-
Contains smooth muscle cells and elastic fibers.
-
Helps control blood pressure and flow by contracting or relaxing.
-
Has an External Elastic Lamina, a less-defined elastic layer.
3. Tunica Adventitia (Outer layer)
-
Made of connective tissue and elastic fibers.
-
Contains nerve fibers and lymphatic vessels.
-
Nourishes the artery wall.
🧪 Nutrient Supply to Arterial Wall
-
Inner layers get nutrients by diffusion from the blood inside the artery.
-
Outer layers are supplied by small blood vessels called vasa vasorum ("vessels of the vessels").
🔬 Structural Changes with Size
-
As arteries become smaller (from large arteries to arterioles), the thickness of all 3 layers decreases.
-
Elastic tissue reduces, and eventually elastic lamina disappears in arterioles.
🧵 Arterioles
-
Very small arteries (20-100 µm).
-
Have thin walls:
-
1 layer of endothelium.
-
1-2 layers of smooth muscle.
-
Minimal connective tissue.
-
-
No visible elastic lamina.
Capillaries
-
Diameter: 7-8 µm (same as a red blood cell).
-
Only one thin endothelial layer.
-
Main site for exchange of gases, nutrients, and waste.
Blood Flow Pathway
Heart ➝ Arteries ➝ Arterioles ➝ Capillaries ➝ Venules ➝ Veins ➝ Heart
🔍 Arteriosclerosis
Arteriosclerosis is a general term used to describe the thickening and hardening of artery walls, leading to reduced elasticity and narrowed blood flow.
💡 Key Term:
-
Arteriosclerosis = Hardening of arteries.
🧠 Types of Arteriosclerosis:
There are four main types:
1️⃣ Senile Arteriosclerosis
Occurs due to aging, affecting many arteries.
🔬 Morphologic Features:
-
Fibroelastosis: Thickening of inner and middle layers due to increased collagen and elastic tissue.
-
Elastic Reduplication: The internal elastic lamina splits, forming two wavy layers.
🩺 Result: Can lead to increased systolic blood pressure in elderly people.
2️⃣ Hypertensive Arteriolosclerosis
Seen in people with high blood pressure (hypertension).
Affects small arteries and arterioles.
💡 3 Types:
i. Hyaline Arteriolosclerosis
-
Walls of arterioles become thick and glassy (hyaline).
-
Lumen becomes narrow or blocked.
🧪 Pathogenesis (Possible Causes):
-
Leakage of plasma proteins due to vessel wall stress.
-
Damage from high blood pressure or diabetes.
-
May also be part of normal aging.
ii. Hyperplastic Arteriolosclerosis
-
Common in malignant (very high) hypertension.
🔬 Morphologic Features:
-
Onion-skin appearance: Multiple layers of smooth muscle cells in the intima.
-
Other types:
-
Mucinous thickening: Deposits of jelly-like substances.
-
Fibrous thickening: Collagen and hyaline material buildup.
-
🧪 Pathogenesis:
Due to endothelial damage caused by high pressure → repair response → thickening.
iii. Necrotising Arteriolitis
-
Seen in severe or malignant hypertension.
🔬 Features:
-
Fibrinoid necrosis: Vessel wall cells die and form debris.
-
Neutrophils: Immune cells infiltrate the area.
-
Surrounding bleeding and swelling.
🧪 Cause:
Sudden spike in blood pressure causing direct injury to vessel walls.
3️⃣ Mönckeberg’s Arteriosclerosis
Also called Medial Calcific Sclerosis.
Affects medium and large muscular arteries, especially in the legs and genital area, usually in people above 50.
💡 Key Points:
-
Calcium is deposited in the media (middle layer).
-
No inflammation.
-
Lumen remains open – blood flow is not affected.
-
Found incidentally on X-rays.
🧪 Cause:
Considered an age-related degenerative change (possibly due to repeated vasoconstriction).
📌 Summary Table:
| Type | Cause | Affected Area | Main Feature |
|---|---|---|---|
| Senile | Aging | Media & Intima | Thickening, elastic changes |
| Hyaline | HTN, Diabetes, Aging | Arterioles | Hyaline material deposits |
| Hyperplastic | Malignant HTN | Intima | Onion-skin smooth muscle |
| Necrotising | Sudden HTN | Arterioles | Fibrinoid necrosis |
| Mönckeberg's | Aging | Media | Calcium deposits, no narrowing |
🧠 Important Terms Explained:
-
HTN = Hypertension = High Blood Pressure
-
Lumen = The hollow space inside a blood vessel
-
Intima/Media/Adventitia = The three layers of the artery wall
-
Fibrinoid Necrosis = Cell death + fibrin-like material in walls
-
Onion-skin lesion = Layered thickening of vessel walls
-
Hyaline = A glassy, pink-staining material seen in tissues
-
Calcification = Deposit of calcium salts in tissue
4. Atherosclerosis
🧬 Definition
Atherosclerosis is a type of arteriosclerosis where fatty plaques (atheromas) develop in the intima (inner lining) of large and medium-sized arteries.
Word origin:
-
Athero- = "gruel" or "porridge" (soft, lipid core)
-
-Sclerosis = "hardening" (fibrous cap and connective tissue)
🫀 Commonly affected arteries:
-
Aorta
-
Coronary arteries
-
Cerebral arteries
-
Peripheral arteries
🚨 Clinical Consequences of Atherosclerosis
Heart:
-
Angina (chest pain)
-
Myocardial infarction (heart attack)
-
Chronic ischemic heart disease
Brain:
-
Transient ischemic attacks (TIAs)
-
Cerebral infarcts (strokes)
-
Ischemic encephalopathy
Other:
-
Peripheral arterial disease
-
Mesenteric ischemia
-
Aneurysm formation
🧾 Etiology (Causes & Risk Factors)
Major Risk Factors
🛠️ Modifiable:
-
Dyslipidemia (abnormal cholesterol/triglycerides)
-
Hypertension (high BP)
-
Smoking
-
Diabetes Mellitus
📌 Non-Modifiable:
-
Age
-
Male gender
-
Genetic predisposition
-
Family history
🌱 Emerging Risk Factors
-
Obesity
-
Lack of exercise
-
Inflammation (high CRP)
-
Stress
-
Hormonal imbalances (e.g. postmenopausal estrogen loss)
-
Infections (e.g. Chlamydia pneumoniae)
💊 Modifiable Risk Factors in Detail
1. Dyslipidemia
Lipoproteins:
-
LDL = “Bad” cholesterol → deposits fat in arteries
-
HDL = “Good” cholesterol → removes fat from arteries
📉 Normal levels:
| Lipid | Normal Range | Risk Impact |
|---|---|---|
| Total Cholesterol | < 200 mg/dL | ↑ = High risk |
| LDL | < 130 mg/dL | ↑ = Very atherogenic |
| HDL | > 60 mg/dL | ↑ = Protective |
| Triglycerides | < 160 mg/dL | ↑ = Risk factor |
🧬 Familial hypercholesterolaemia:
-
Genetic condition
-
↑ LDL
-
Normal triglycerides
-
Early atherosclerosis and heart attacks
Management:
-
Diet & exercise
-
Statins
-
HDL boost with niacin
2. Hypertension
Blood pressure >160/95 mmHg:
-
Causes mechanical stress on artery walls
-
↑ Risk by 5x
🎯 Goal BP: <140/90 mmHg
3. Smoking
-
Decreases HDL, increases clotting
-
Forms carboxyhemoglobin → ↓ oxygen to arterial walls
-
Causes hypoxia and injury
-
3–5x ↑ risk of heart disease
4. Diabetes Mellitus
-
Type 2 diabetes strongly linked to atherosclerosis
-
Common complications:
-
Double risk of heart attack
-
Higher stroke risk
-
🦶 100x ↑ risk of gangrene
-
📜 Constitutional (Non-Modifiable) Risk Factors
Age
-
Lesions start early (even in childhood), worsen with age
Gender
-
Males > Females (before menopause)
-
Estrogen is protective
Genetics & Race
-
Family history increases risk
-
Some racial groups more prone (e.g. South Asians)
🌱 Emerging Risk Factors in Atherosclerosis
These are nontraditional and newly recognized factors whose role in causing atherosclerosis is not yet fully established, but evidence is growing.
1. Environmental Influence
Higher incidence in developed countries suggests environmental and lifestyle factors (e.g., diet, pollution, urban stress) contribute to disease.
2. Obesity
If body weight is 20% or more above ideal, the risk of atherosclerosis significantly increases.
📈 Obesity is linked with:
-
↑ LDL
-
↓ HDL
-
Insulin resistance
-
Inflammation
3. Hormonal Factors
-
Exogenous hormones (e.g., oral contraceptives)
-
Endogenous estrogen deficiency in post-menopausal women
🔺 Associated with increased risk of heart attacks and strokes
4. Physical Inactivity
Sedentary lifestyle & lack of exercise increases the chance of:
-
Obesity
-
Dyslipidaemia
-
Insulin resistance
-
Endothelial dysfunction
Regular activity improves vascular health and lipid profile
5. Stress & Personality Type
People with “Type A” personality (aggressive, competitive, time-urgent) are at greater risk of Ischemic Heart Disease (IHD) compared to “Type B” (relaxed, easygoing).
🧠 Stress hormones (like cortisol, adrenaline) may damage blood vessels over time.
6. Homocystinuria
A rare inborn error of metabolism
⚠️ Patients have high homocysteine levels → linked to early atherosclerosis and coronary artery disease
7. Prothrombotic State
-
Elevated fibrinogen levels
-
Other clot-promoting substances
🧨 These factors can trigger thrombus formation, the most dangerous complication of atherosclerosis.
8. Infections
Pathogens found in atherosclerotic plaques:
-
Chlamydia pneumoniae
-
Herpesvirus
-
Cytomegalovirus (CMV)
They may promote inflammation and plaque instability, often in synergy with other risk factors.
9. Markers of Inflammation
C-Reactive Protein (CRP) – an acute phase reactant
📊 High CRP levels = higher risk of developing or worsening atherosclerosis
🧠 Inflammation plays a central role in atheroma formation and rupture.
🩺 Pathogenesis
Accepted steps in the development of atherosclerosis.
🩹 1. Endothelial Injury – The First Trigger
-
Endothelial dysfunction, not necessarily full denudation (loss or stripping away of a surface layer), initiates plaque formation.
-
Causes in animals:
-
Mechanical trauma
-
Hemodynamic forces
-
Chemical/toxic agents
-
Metabolic conditions (e.g., dyslipidemia, homocysteine)
-
Infections, toxins, tobacco, radiation
-
-
💡 Plaques commonly form at arterial branches due to high shear stress
🧬 2. Intimal Smooth Muscle Cell Proliferation
-
Endothelial injury → platelet adhesion + inflammation → smooth muscle cell proliferation
-
Stimulated by cytokines: IL-1, TNF-α (from invading monocyte-macrophages and
by activated platelets)
-
Key growth factors:
-
PDGF, FGF → migration & proliferation of smooth muscle cells into intima
-
TGF-β, IFN-γ → regulate collagen synthesis
-
-
Molecules involved: Nitric oxide, Endothelin (from endothelium)
-
Smooth muscle cells produce matrix proteins: Collagen, Elastic fibers, and Proteoglycans
🧲 3. Role of Blood Monocytes
-
Plasma LDL enters intima and undergoes oxidation → becomes oxidized LDL
-
Oxidized LDL functions:
-
Attracts & activates monocytes
-
Taken up by scavenger receptors on monocytes → transforms into foam cells
-
-
Oxidized LDL is toxic to endothelium
-
Foam cells undergo apoptosis, releasing lipids → form lipid core of plaque
🧪 4. Role of Dyslipidaemia
-
Chronic dyslipidemia promotes endothelial dysfunction and increases permeability
-
LDL (bad cholesterol) → forms foam cells
-
HDL (good cholesterol) → anti-atherogenic (protective)
🩸 5. Thrombosis – Final Plaque Evolution
-
Endothelial damage exposes subendothelial connective tissue → triggers:
-
Platelet aggregation
-
Smooth muscle proliferation
-
-
Small platelet clots + inflammation + foam cells = atheromatous plaque
-
Fibrin and circulating cells may attach to lesion → thrombus becomes part of plaque
Morphologic Features of Atherosclerosis
🟡 1. Fatty Streaks & Dots
-
Seen in infancy, regress with age.
-
Location: Posterior aorta
-
Microscopy: Foam cells, lipid-rich SMCs, ECM, few lymphocytes.
🌫 2. Gelatinous Lesions
-
Grey, raised, round/oval lesions (~1cm).
-
Histology: Increased ground substance + thinned endothelium.
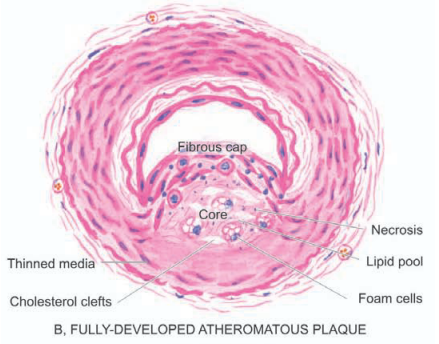
⚪️ 3. Atheromatous Plaques (Fibrous/Fibrofatty Plaques, Atheromas)
-
Common in elderly, advanced lesions.
-
Locations:
-
Abdominal aorta
-
Coronaries, carotids, cerebrals, femoral, iliac arteries.
-
-
Gross: White/yellow, raised plaques with firm fibrous cap and soft yellow core.
-
Microscopy:
-
Fibrous cap: SMCs, collagen, proteoglycans, endothelium.
-
Cellular layer: Macrophages, lymphocytes, foam cells.
-
Core: Necrosis, cholesterol clefts, fibrin, lipid debris.
-
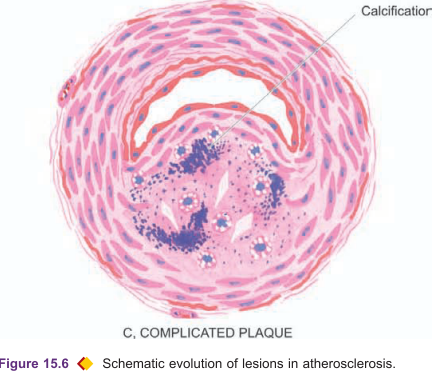
⚠️ 4. Complicated Plaques
i) Calcification
-
Eggshell-like cracking in aorta/coronaries.
-
Histology: Calcium near necrotic/lipid zones.
ii) Ulceration
-
Rupture of fibrous cap → Lipid emboli → Yellow ulcer base.
-
Can lead to sudden coronary occlusion.
iii) Thrombosis
-
Over ulcerated plaques → Mural thrombi or occlusion.
-
May become emboli or undergo recanalization.
iv) Hemorrhage
-
Source: Ulceration or vasa vasorum rupture.
-
Common in coronaries.
-
Macrophages with hemosiderin present.
v) Aneurysm Formation
-
Media atrophy, fragmented elastic lamina.
-
Adventitial fibrosis → Wall weakening → Dilatation.
🏥 3. Clinical Effects of Atherosclerosis
General Effects
-
Chronic ischemia → Atrophy
-
Acute occlusion → Infarction
-
Thromboembolism
-
Aneurysm + rupture
Organ-Specific Outcomes
-
Aorta: Aneurysms, thrombi, emboli
-
Heart: MI, ischemic heart disease
-
Brain: Infarcts, chronic ischemia
-
Intestines: Ischemic bowel, infarction
-
Lower limbs: Intermittent claudication, gangrene
ARTERITIS (Angiitis / Vasculitis)
Definition:
Arteritis refers to inflammation of arteries or arterioles. It is also known as angiitis or vasculitis and may result from infectious or non-infectious causes. The non-infectious causes are more common clinically.
CLASSIFICATION OF ARTERITIS:
| Type | Description |
|---|---|
| I. Infectious Arteritis | Caused by direct microbial invasion (bacteria, fungi) or hematogenous spread of infection. |
| II. Non-infectious Arteritis | Caused by immune-mediated, chemical, mechanical, or radiation-induced injury. |
I. INFECTIOUS ARTERITIS
1. Endarteritis Obliterans
-
Definition: A non-specific response of arteries to chronic irritation (not a true inflammatory disease).
-
Associated with: Peptic ulcers, TB, chronic abscesses, meningitis, postpartum/postmenopausal uterus.
-
Gross: Lumen may appear normal externally but show luminal obliteration (a condition where the interior space of a tubular structure, such as a blood vessel or organ duct, is completely blocked or closed off) on section.
-
Microscopy:
-
Intimal fibrosis with concentric, symmetrical fibrous tissue proliferation.
-
Minimal or no inflammation, despite the “-itis” suffix.
-
2. Non-Syphilitic Infective Arteritis
-
Causes: Bacterial, fungal, parasitic, or viral infections via direct or hematogenous routes.
-
Microscopy:
-
Inflammatory infiltrate in vessel walls.
-
Lumen occlusion by thrombi → ischemic necrosis of supplied tissue.
-
3. Syphilitic Arteritis
-
Occurs in all stages of syphilis, especially the tertiary stage.
-
Two forms:
-
Endarteritis (arterial wall)
-
Periarteritis (periarterial tissue)
-
-
Common sites: Aorta and cerebral arteries
A. Syphilitic Aortitis
-
Location: Most commonly affects ascending aorta and aortic arch.
-
Gross Features:
-
Aorta appears dilated and thickened.
-
"Tree-bark" appearance: Intimal surface with pearly-white plaques separated by wrinkled areas.
-
-
Microscopy:
-
Endarteritis and periarteritis of vasa vasorum in the media and adventitia.
-
Perivascular plasma cells, lymphocytes, macrophages ± miliary gummas.
-
Intimal fibrosis, collagenous, often hyalinized or calcified.
-
-
Consequences:
-
Aortic aneurysm.
-
Aortic valvular incompetence (rare today).
-
Coronary ostial stenosis → myocardial fibrosis, angina, sudden death.
-
B. Cerebral Syphilitic Arteritis (Heubner’s Arteritis)
-
Involves small and medium cerebral arteries in tertiary syphilis.
-
Often coexists with syphilitic meningitis.
-
Gross: Thickened, rigid, white cerebral vessels.
-
Microscopy:
-
Endarteritis and periarteritis.
-
Medial muscle atrophy replaced by fibrosis → brain ischemia and atrophy.
-
non-infectious vasculitides
Polyarteritis Nodosa (PAN)
-
Type: Necrotizing vasculitis of small and medium-sized muscular arteries.
-
Etiology: Immune complex-mediated; triggered by infections (HBV, bacteria), drugs, etc.
-
Organs Affected: Kidneys, heart, GI tract, muscles, liver, nerves, testes, skin.
-
Clinical Features:
-
Fever, malaise, weight loss
-
Renal involvement: proteinuria, hematuria, renal failure
-
GI symptoms: abdominal pain, melena
-
Peripheral neuritis, hypertension
-
-
Gross: Beaded nodules at vessel bifurcations
-
Microscopy:
-
Acute: Fibrinoid necrosis, neutrophils/eosinophils, thrombi, aneurysms
-
Healing: Fibroblast proliferation, lymphocytes, plasma cells
-
Healed: Dense fibrosis, loss of internal elastic lamina
-
Hypersensitivity Vasculitis (Microscopic Polyangiitis)
-
Also Known As: Allergic vasculitis, leukocytoclastic vasculitis
-
Vessels Affected: Venules, capillaries, arterioles (small vessels)
-
Causes: Infections, drugs, autoimmune diseases (RA, SLE), malignancies
-
Organs Affected: Skin, mucosa, lungs, brain, heart, kidneys
-
Microscopy:
-
Leukocytoclastic: Fibrinoid necrosis, neutrophilic debris
-
Lymphocytic: Lymphocyte-dominant; delayed-type hypersensitivity
-
Wegener’s Granulomatosis (Granulomatosis with Polyangiitis)
-
Triad:
-
Necrotizing granulomas (upper & lower respiratory tract)
-
Necrotizing vasculitis (lungs, airways)
-
Glomerulonephritis (focal or diffuse)
-
-
Organs Affected: Lungs, kidneys, sinuses, joints, skin, eyes, heart, CNS
-
Etiology: c-ANCA (anti-PR3)
-
Histology:
-
Granulomas: necrosis, neutrophils, epithelioid & giant cells
-
Vasculitis: segmental or circumferential
-
Kidney: necrotizing glomerulonephritis
-
Temporal (Giant Cell) Arteritis
-
Type: Granulomatous arteritis of large and medium arteries
-
Common Sites: Temporal artery, aorta, carotids, subclavian
-
Demographic: Elderly (>70), females > males
-
Symptoms: Headache, visual loss, jaw claudication, polymyalgia rheumatica
-
Histology:
-
Granulomatous inflammation around internal elastic lamina
-
Giant cells, fragmentation of lamina
-
Intimal thickening and luminal narrowing/thrombosis
-
Takayasu’s Arteritis (Pulseless Disease)
-
Type: Granulomatous vasculitis of large arteries (mainly aorta and branches)
-
Demographic: Young women
-
Symptoms: Absent upper limb pulses, ocular issues, ischemia-related symptoms
-
Gross: Thickened aortic wall, obliterated lumina
-
Histology:
-
Panarteritis with mononuclear cells
-
Perivascular inflammation of vasa vasorum
-
Granulomas with necrosis, giant cells
-
Advanced fibrosis
-
Kawasaki Disease (Mucocutaneous Lymph Node Syndrome)
-
Demographic: Infants and young children
-
Features:
-
Fever, conjunctivitis, oral erosions, skin rash, cervical lymphadenopathy
-
-
Complications: Coronary artery aneurysms (major cause of pediatric heart disease)
-
Etiology: Unknown (possible infection, autoimmune, genetic)
-
Vessels: Coronary, renal, hepatic, mesenteric, pancreatic arteries
Key Immunologic Markers in Vasculitis
-
c-ANCA (anti-PR3): Wegener’s granulomatosis
-
p-ANCA (anti-MPO): Microscopic polyangiitis, glomerulonephritis
-
AECAs: Kawasaki disease, SLE, Buerger’s disease
-
Pauci-immune: Few/no immune deposits despite vasculitis (e.g., ANCA-associated types)
ANEURYSMS
📘 Definition
Permanent abnormal dilatation of a blood vessel due to congenital or acquired weakening/destruction of vessel wall. Common in large elastic arteries like the aorta. Can lead to thrombosis, rupture, embolism or compression of nearby structures
🗂️ Classification
A. Based on Wall Composition
True Aneurysm – All layers of the vessel wall involved
False Aneurysm – Wall composed of fibrous tissue (often post-trauma)
B. Based on Shape
Saccular – Large, spherical outpouching
Fusiform – Spindle-shaped dilatation
Cylindrical – Continuous, parallel dilatation
Serpentine/Varicose – Tortuous dilatation
Racemose/Circoid – Mass of intercommunicating small vessels
C. Based on Pathogenesis
Atherosclerotic – Most common; related to plaque buildup
Syphilitic (Luetic) – Tertiary syphilis affecting thoracic aorta
Dissecting – Blood enters vessel wall layers
Mycotic – Due to microbial infection
Berry – Found in circle of Willis (brain base)
Atherosclerotic Aneurysms
Pathogenesis
Atherosclerosis causes medial thinning and destruction
Weakening of the wall leads to dilation
Morphologic Features
Commonly infra-renal aorta
Usually >5–6 cm, mostly fusiform
Wall with fibrous tissue; mural thrombus may be present
Effects
Rupture – Risk increases with size/duration
Compression – Can affect ureters, vertebrae
Arterial Occlusion/Thromboembolism – Common complication
Syphilitic (Luetic) Aneurysms
Pathogenesis
Seen in tertiary syphilis (~10% cases)
Inflammatory infiltrate → endarteritis obliterans → media damage
Morphologic Features
Affects ascending aorta/aortic arch
Saccular aneurysms, 3–5 cm
Tree-bark intimal appearance
May cause ‘cor bovinum’ from LV hypertrophy
Effects
Rupture – Fatal hemorrhage into body cavities
Compression – Dysphagia, hoarseness, bone erosion
Cardiac Dysfunction – Aortic incompetence, coronary narrowing
Dissecting Aneurysms (Dissecting Hematoma)
Pathogenesis
Media weakening is key cause
Initiated by intimal tear or vasa vasorum hemorrhage
Risk factors:
-
Hypertension (90% cases)
-
Marfan’s syndrome
-
Iatrogenic trauma
-
Pregnancy
🩸 VEINS – NORMAL STRUCTURE
-
Vein walls are thinner than arteries.
-
Elastic tissue is scanty; no clear elastic laminae.
-
Sparse smooth muscle; collagen-rich media.
-
Valves prevent backflow—best developed in leg veins.
🪢 VARICOSITIES
-
Abnormally dilated & twisted veins.
-
Common Locations:
-
Legs → Varicose veins
-
Esophagus → Esophageal varices
-
Anus → Hemorrhoids
-
Spermatic cord → Varicocele
-
🧵 VARICOSE VEINS
-
Definition: Permanently dilated, tortuous superficial leg veins.
Peak: 40s–50s
More common in women (especially during pregnancy)
-
Causes:
-
Genetic weakness of valves/walls
-
Prolonged standing (e.g., nurses, surgeons)
-
Pregnancy (compression on iliac veins)
-
Hormonal effects
-
Obesity
-
Constipation
-
-
Pathology:
-
Dilated, nodular veins
-
Fibromuscular wall thickening
-
Elastic degeneration, thrombosis
-
-
Effects:
-
Venous stasis → congestion, edema
-
Thrombosis, dermatitis, cellulitis
-
Chronic varicose ulcers
-
🧬 PHLEBOTHROMBOSIS & THROMBOPHLEBITIS
-
Phlebothrombosis: Clot in vein
-
Thrombophlebitis: Inflammation of vein
-
Causes (Virchow's Triad):
-
Endothelial injury
-
Hypercoagulability
-
Venous stasis
-
-
Risk Factors:
-
Heart failure
-
Cancer
-
Estrogens
-
Post-surgery
-
Immobility
-
MORPHOLOGY
-
Gross: Normal or distended veins with thrombus
-
Histology: Intimal inflammation → fibroblast response → fibrosis or resolution
CLINICAL EFFECTS
-
Local: Swelling, pain, redness, heat
-
Systemic:
-
Pulmonary embolism (most common)
-
Septic emboli to brain/liver/meninges
-










Comments
Post a Comment